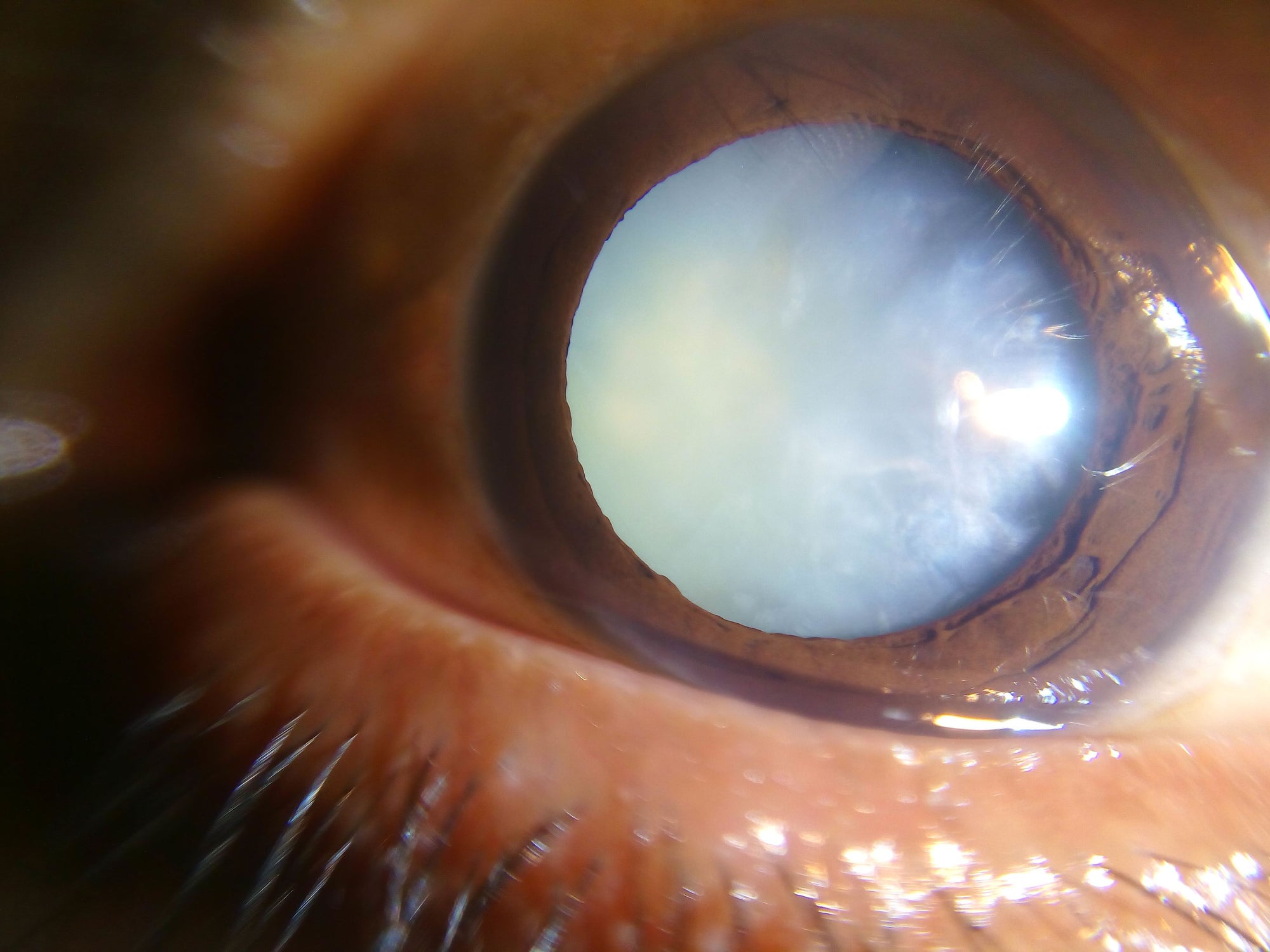
Most of the time, cataract surgery is an easy, comfortable and fast surgery for patient and surgeon alike. Modern techniques often use femtosecond laser to divide the cataract into manageable pieces and create computer-perfect tissue incisions.
But other times, cataract surgery is anything but routine.
In a recent surgery, I treated a patient with ankylosing spondylitis, an auto-immune rheumatologic condition, associated with Human Leukocyte Antigen B-27, and which can cause severe deformities of the cervical spine.
In this case, his neck was permanently flexed in a frozen position nearly 90 degrees from the rest of the spine. Meanwhile, cataract surgery requires that the face be nearly parallel to the floor, in order to align with the microscope.

By putting him in a Trendelenburg position, which is normally used for abdominal surgery, with his body up in the air, strapped tightly to the bed, we were able to nearly but not completely get his face in the correct position. But that left his head completely unsupported. And to rectify that, we ultimately used an additional bed, placed at a right angle underneath his head.
The head of the bed was so close to the ground that I could not place my legs underneath, and had to put them to my left side and twist my body to the right to perform the surgery.
There are many other situations that make cataract surgery anything but routine, including:
- Pseudoexfoliation Syndrome
- Concomitant Glaucoma
- Small Pupil Size
- Floppy Iris Syndrome from Flomax
- Small or Large Eye
- Corneal Scarring
- Narrow Anterior Chamber Angle of the Eye
- Iris Scarring
- Marfan's Syndrome
- Prior Retinal Detachment
- History of Uveitis