Prednisone, a glucocorticoid, is used to treat a number of diseases, some acutely (asthma suddenly out of control), some chronically (ulcerative colitis, Polymyalgia rheumatica, Giant Cell Arteritis). Despite the plethora of powerful new medications being developed, prednisone still works well to control the inflammation of a number of illnesses and diseases better than the modern alternatives. The problems arise when the side effects begin to take effect. And the side effects with prednisone are many. They include: brittle bones (osteoporosis), which can increase the risk of bone fractures and spinal pain, increased weight, elevated blood sugar, and increased risk of infection. But ocular side effects can reduce vision, and in some cases, cause blindness.
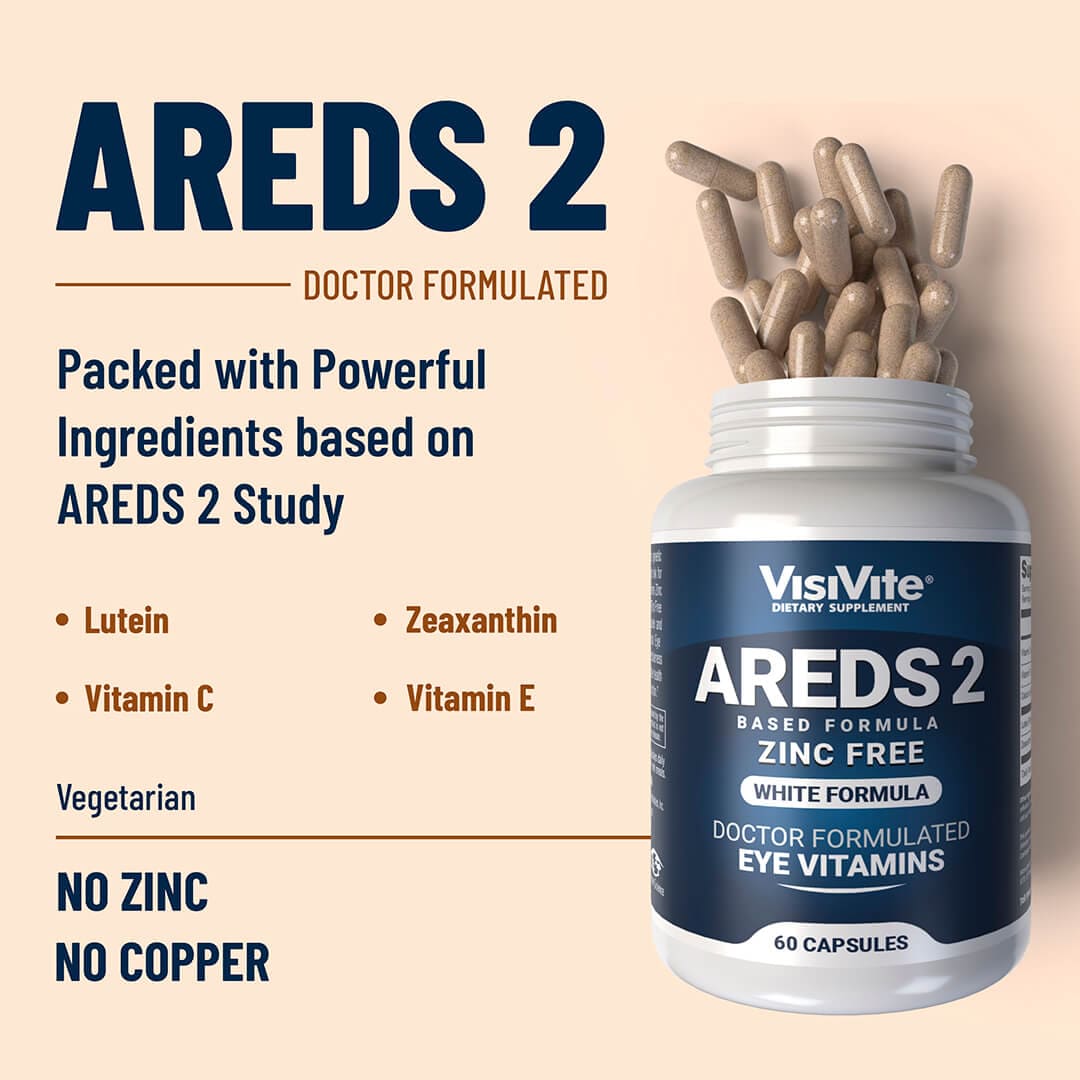
[caption id="" align="alignleft" width="262"] Prednisone may cause cataract formation[/caption]
Prednisone causes the formation, in many people of a type of lens opacification known as posterior subscapsular cataracts. These cataracts, known as "PSC's" by ophthalmologists, are particular visually debilitating because the loss in lens clarity occurs in the back of the lens, which is the optical center of the lens where all light travels before heading to the retina in the back of the eye. Symptoms include glare and halos and difficulty reading details up close. This latter effect occurs due to the pupil constricting during reading, which forces light to travel through the most opaque portion of the cataract.
But cataracts are not the only side effect from Prednisone. Elevation in eye pressure may also occur, above and beyond the upper normal limit of 21 mm Hg. Patients may assume that taking oral prednisone for only one or two months could not possibly be harmful, and their doctors are often unaware of the rapid rise in pressure to levels of 30 to 50 mm Hg that can occur in people who have diabetes, those with a family history of glaucoma, or those people who have a borderline pressure level to begin with. Approximately 10% of people are "steroid responders," who develop elevated intraocular pressures in response to oral prednisone.
Patients often ask whether nasal or oral steroid inhalers can also raise pressure. The answer is yes, but rarely. The culprit is almost always oral steroids, or steroid eyedrops themselves.
If you listen to the commercials on television and radio, you'll undoubtedly hear about other drugs that "can cause glaucoma," but are really rather rare. These include all drugs with "anticholinergic side effects," and include such common drugs as cold remedies and spastic bladder medications.
Although these are very common telephone inquiries to an eye doctor, in fact the incidence of developing glaucoma is rare.
Why?
Because these medications dilate the pupil slightly, which increases the risk of an angle closure glaucoma attack in patients with narrow anterior chamber angles, but have no effect on nearly everyone else, including those patients with the most common form of glaucoma, known as primary open angle glaucoma.
So why do the ads warn against taking the medications if you have, "glaucoma?" Read the previous paragraph and decide for yourself which saves the advertiser the most time (and dollars) in their ads.
Yep. "Don't take the meds if you have glaucoma," saves the advertisers money, even though it is an inaccurate statement.
There is another medication that requires frequent monitoring. Plaquenil (hydroxychlorquine) is used to treat Rheumatoid arthritis and other "autoimmune" diseases. An infrequent, but serious side effect is the loss of scattered areas of the vision that might not be detected using a simple eye chart test. The recommended test is a computerized visual field examination, which assesses for loss of tiny areas of peripheral, or "side vision." Often seen concomitantly with the visual field loss is a retinal finding known as Bull's Eye Maculopathy. The finding of either visual field loss or Bull's Eye Maculopathy warrants the discontinuation of hydroxycholoroquine.
Medications that are used to treat erectile dysfunction may cause the user to see a blue haze in their vision. While alarming, however, this transient visual change does not appear to induce any permanent damage.
And finally, no discussion of ocular side effects of prescription medications would be complete without discussing prostate medications. The worst of the bunch seems to be Flomax, a drug that blocks the alpha adrenergic receptors not just surrounding the prostate, but everywhere else in the body too. I have previously written about this in greater detail on the page explaining causes of Floppy Iris Syndrome. In short, the medication causes the iris dilator muscle to relax, sometimes permanently. This results in a small pupil, again sometimes permanently. A small pupil is not in itself, a dangerous thing. But a small pupil, particularly with a floppy iris, makes cataract surgery more difficult. I perform nearly 600 cataract surgeries annually. Among that number are eye doctors who refer me their patients who have taken Flomax and are at high risk for Floppy Iris Syndrome. Despite my expertise in treating patents with Floppy Iris Syndrome, I would much prefer if the patient had not taken Flomax or another alpha adrenergic drug prior to cataract surgery.
If your doctor is considering using Flomax to treat your prostate hyperplasia, my recommendation is to go to your eye doctor first to be evaluated for cataract surgery. It is much more desirable to do the cataract surgery first, and THEN AFTERWARDS, start the Flomax regimen.
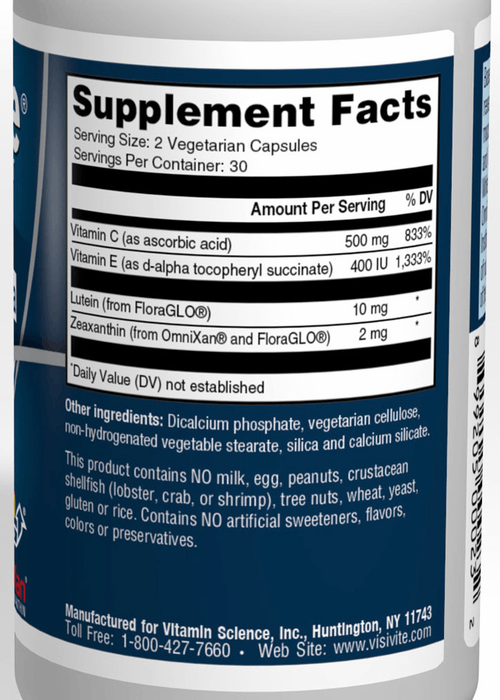
Paul Krawitz, M.D., President
Vitamin Science, Inc.